I normally write blog posts about education, or things that are generally enjoyable to me, seeing the panic and economic hardship due to SARS CoV-2 (coronavirus) is not enjoyable to me, but alas it has gripped the attention of the world. I see the news and I see political leaders talk; I see massive closures of businesses, schools, public gatherings, and even small gatherings of more than 5 people. A lot have been talking about the transmission of SARS CoV-2 and the impact it has had, I personally have been wondering the transmission of information in this current time.

For some reason, I had to go a little bit deeper, and with full disclosure, I am not a medical expert, medical researcher, epidemiologist, biochemist, virology expert, or hold any sort of medical doctorate or licence to practice medicine. But I am currently a masters student engaging in research, certified TCPS 2 Ethical Researcher, and I enjoy doing Systematic Literature Reviews (SLR). With the current resources at my disposal, I decided to look for research articles pertaining to SARS CoV-2 to obtain information and what the scientific community says regarding this virus.
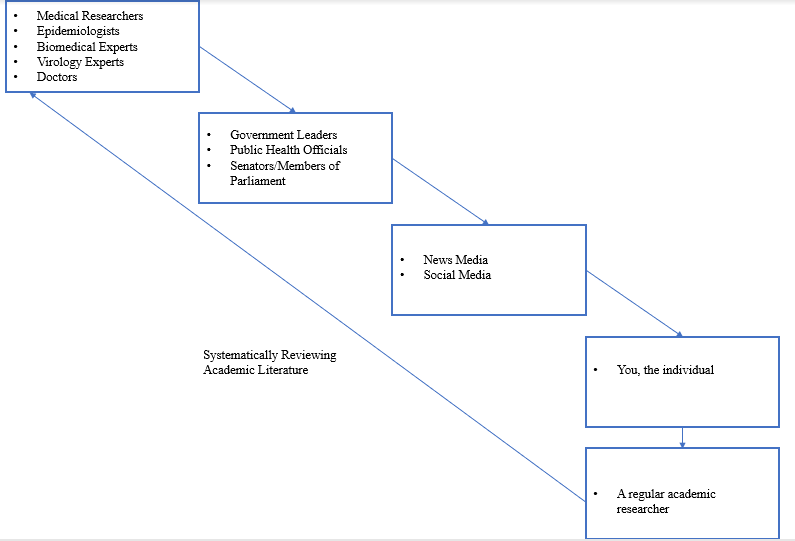
Review Process
I have my ideas regarding the fear and panic about this virus and what I hope for is to gain clarity from this. I want to see if I am justified or unjustified in my feeling towards the SARS CoV-2 panic and fear. The point of research is not to prop your own ideas, it is to objectively look at the data presented and make a judgement relying on that data. With that, here is the list of articles and how I obtained them.
First Review
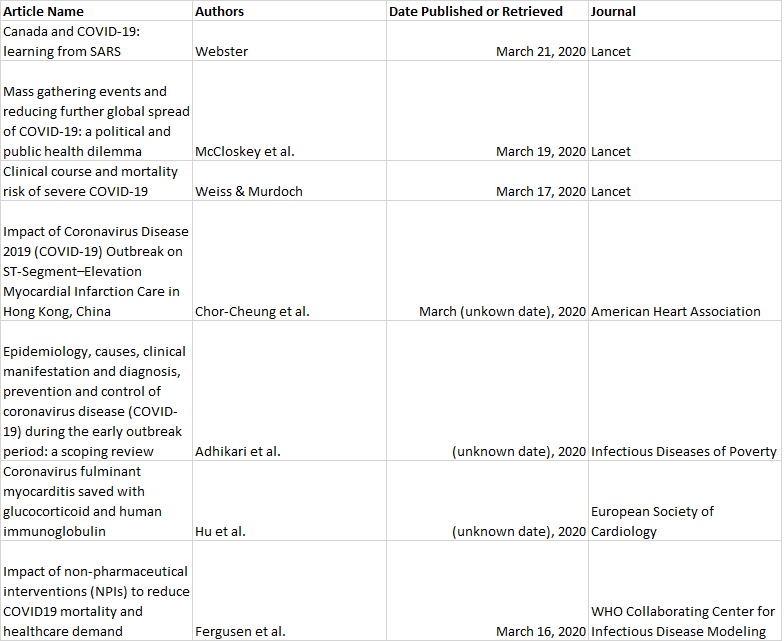
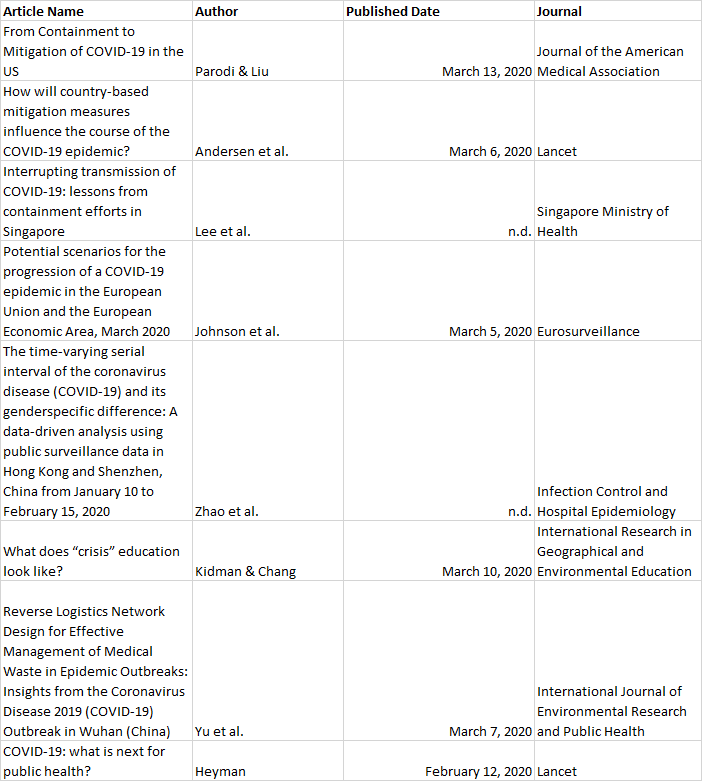
This took place by looking at the current research articles accepted by the World Health Organization (WHO) relating to SARS CoV-2. I was directed to an excel spreadsheet where hundreds of articles were presented. I went through over 70 articles finding nine with current relevancy to what I felt discussed the disease and mitigation of.
Second Review
The second review used my university’s library database and Boolean Search Parameters to find articles relating to COVID-19 and mitigation. Placing active search filters for Peer-reviewed journal articles, the following articles emerged.
Data Analysis
From what the research provided, I was able to get a grasp on a host of information. First, it seems clear that the research shows 80-81% of individuals who will contract COVID-19 will show mild symptoms or be completely asymptomatic (Anderson et al., 2020; Weiss & Murdoch, 2020), and although all ages can contract the disease, the most at risk are the elderly (median age 75), immuno-comprimized, users of immunosuppresive agents, serious surgical history and patients who are at risk for ST-Elevation Myocardial Infarction (STEMI) (Adhikari, et al., 2020; Chor-Cheung et al., 2020; Hu, et al. 2020).
One significant theme through the research is the general “R Naught” or “R0” which is the basic reproductive number of the virus. Some research suggested R0 in between 1-1.5 to 2-5 depending on the virology count. Andersen (2020) suggests that if the R0 remains low, warm weather can have an impact on the virus, much like influenza, however of an R0 of 2-3 or higher, warm weather will not have an impact.
Social Measures: Suppression vs. Mitigation
Most articles discussed social measures by governments and public health institutions can pursue in this pandemic. Many researchers cited public policy makers and governments leaning on inconsistencies towards their suppression or mitigation by not taking in multiple factors when making decisions (McCloskey, et al., 2020; Webster, 2020). Furthermore, Kidman and Chang (2020) outline precarious information being presented on social media, and mainstream media having an impact on community decisions.
Research suggests that communities do take up action with social distancing and quarantine for at risk members of society and individuals who contracted COVID-19, without mass shutdowns, such as schools and businesses (Adhikari, et al., 2020; Ferguson, et al., 2020; Parodi & Liu, 2020). This is reflected in the Singapore model where confirmed cases were placed in immediate quarantine and social responsibility was in place with cleanliness and sanitation with no school closures no business closures and no major social distancing measures (Lee et al., 2020).
Ferguson et al. (2020) provides a graph on mitigation relating to strain on the medical system relating to the different mitigation measures, they are listed as follows:
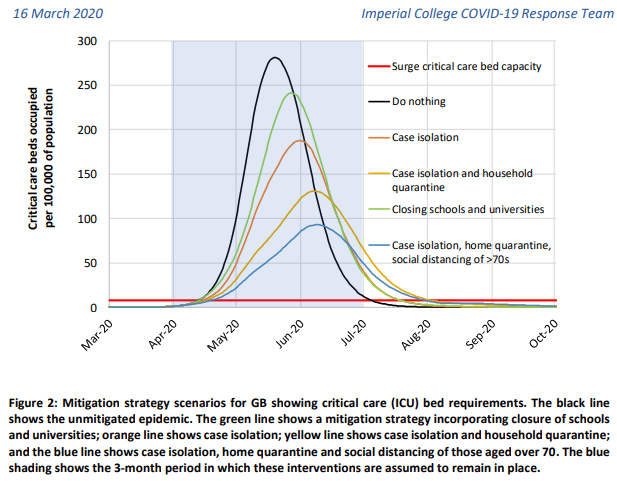
What is reflected here is the measure of ‘doing nothing’ provides a definite spike in cases and a potential burden of the healthcare system, but a significant and quicker drop off. However, measures where case isolation of at-risk populations are presented provides the best measure to lower cases and burden on a health care system (Ferguson, et al., 2020), but drop off is longer. If we look at Canada now, we are somewhere in the middle of the yellow line and the green line as we have closed schools and case isolation with wide household quarantine. Please also note, this graph is a model not an exact representation of numbers, given Ferguson et al. does not have that information.
Further Considerations
It is also important to point out that significant research suggest that school closures are not a significant measure to lowering the curve of the virus (Andersen et al. 2020; Ferguson et al., 2020; Kidman & Chang, 2020). In addition, better support and management needs to be provided for hospital work including medical sanitation, effective mitigation management, and statistical control measures (such as the lowering serial intervals in patients) to manage and inform effectively, not overburden the healthcare system or the economy (Heymann & Shindo, 2020; Johnson, et al, 2020; Yu et al., 2020; Zhao, et al. 2020).
Personal Reflection
It is Andersen that suggests that governments and policy makers need to take a pragmatic approach to social distancing to ensure proper mitigation of COVID-19. The question I propose to Canadians (or where ever your home country is), have your public leaders taken a pragmatic approach to social distancing, and mitigation of COVID-19? And, what are the current motives of social and mainstream media during this pandemic, is it justified? There may be some room for criticism there especially coming from social and mainstream media outlets and the public perceptions leading to socio-economic, and political influence.
My final conclusions from this literature review show:
- Social distancing and quarantine is a highly-beneficial measure for members who are at risk (elderly, immunocompromised, congenial heart issues, chronic co-morbility, etc.) through case by case isolation.
- The closing of schools does not mitigate the threat of COVID-19.
- Like Singapore, we must practice social responsibility at schools, in the workplace and out in public. Much like the WHO and CDC guidelines of wash hands frequently, stay home if you feel ill, cough and sneeze into your arm or a tissue, and be cognizant of social distancing measures.
- Economic issues will continue with drastic quarantine measures.
As a final caveat, I AM NOT A VIROLOGY, EPIDEMIOLOGY, MICROBIOLOGY EXPERT, NOR DO I HOLD ANY ACADEMIC OR PROFESSIONAL CERTIFICATION TO PRACTICE MEDICINE. I simply just read what is available to me, synthesize the linguistic data and make conclusions based on the data. If you have access, you are allowed to view my references down below. It is clear you might have a different take on the information and I welcome that.
I sure do hope as we move forward, government leaders and public institutions will take a more pragmatic and rational approach with a return to normalcy. We want to mitigate the threat of COVID-19 as much as possible, so lets actually take a look a deeper look and adjust accordingly.
References
Adhikari, S. P. et al. (2020). Epidemiology, causes, clinical manifestation and diagnosis, prevention and control of coronavirus disease (COVID-19) during the early outbreak period: a scoping review. Infectious Diseases of Poverty, 9(29), 1-12.
Andersen, R. M. et al. (2020). How will country-based mitigation measures influence the course of the COVID-19 epidemic? The Lancet, 395, 931-934. https://www.thelancet.com/action/showPdf?pii=S0140-6736%2820%2930567-5
Chor-Cheung, F. T. et al. (2020). Impact of Coronavirus Disease 2019 (COVID-19) Outbreak on ST-Segment–Elevation Myocardial Infarction Care in Hong Kong, China. American Heart Association.
Ferguson, N. M. et al. (2020). Impact of non-pharmaceutical interventions (NPIs) to reduce COVID19 mortality and healthcare demand. World Health Organization Collaborating Center for Infectious Disease Modeling and Imperial College of London. https://www.imperial.ac.uk/media/imperial-college/medicine/sph/ide/gida-fellowships/Imperial-College-COVID19-NPI-modelling-16-03-2020.pdf
Heymann, D. L., & Shindo, N. (2020). COVID-19: what is next for public health? The Lancet, 395, 542-545. https://www.thelancet.com/action/showPdf?pii=S0140-6736%2820%2930374-3
Hu, H. et al. (2020). Coronavirus fulminant myocarditis saved with glucocorticoid and human immunoglobulin. European Society of Cardiology.
Johnson, H. C. et al. (2020). Potential scenarios for the progression of a COVID-19 epidemic in the European Union and the European Economic Area, March 2020. Eurosurveillance, Europes Journal on Infectious Disease Epidemiology.
Kidman, G., & Chang, C. H. (2020). What does “crisis” education look like? International Research in Geographical and Environmental Research, 29(2), 107-111.
Lee, V. J. et al. (2020). Interrupting transmission of COVID-19: lessons from containment efforts in Singapore. Ministry of Health, Singapore.
McCloskey, B. et al. (2020). Mass gathering events and reducing further global spread of COVID-19: a political and public health dilemma. The Lancet, 1-3. https://www.thelancet.com/action/showPdf?pii=S0140-6736%2820%2930681-4
Parodi, S. M., & Liu, V. X. (2020). From Containment to Mitigation of COVID-19 in the US. Journal of the American Medical Association. https://jamanetwork.com/journals/jama/fullarticle/2763187
Webster, P. (2020). Canada and COVID-19: Learning from SARS. The Lancet, 395, 936-937. https://www.thelancet.com/action/showPdf?pii=S0140-6736%2820%2930670-X
Weiss, P., & Murdoch, D. R. (2020). Clinical course and mortality risk of severe COVID-19. The Lancet, 1-2. https://www.thelancet.com/action/showPdf?pii=S0140-6736%2820%2930633-4
Yu, H. et al. (2020). Reverse logistics network design for effective management of medical waste in epidemic outbreaks: Insights from the coronavirus disease 2019 (COVID-19) outbreak in Wuhan (China). International Journal of Environmental Research and Public Health, 17, 1-25.
Zhao, S. et al. (2020). The time-varying serial interval of the coronavirus disease (COVID-19) and its gender specific difference: A data-driven analysis using public surveillance data in Hong Kong and Shenzhen, China from January 10 to February 15, 2020. Infection Control and Hospital Epidemiology.

4 thoughts on “Finding a rational middle: Objective and systematic literature review of SARS CoV-2 research articles.”